Mohamad-Ali Salloum is a Pharmacist and science writer. He loves simplifying science to the general public and healthcare students through words and illustrations. When he's not working, you can usually find him in the gym, reading a book, or learning a new skill.
Why ACE inhibitors cause cough?
Share
In this article, I will go briefly through the indications of ACEi and the background of this topic. Then I will discuss the mechanism of cough induction and how to clinically manage the patient. And lastly I will talk about interesting results from 2 studies.ACE inhibitors.
ACE is the abbreviation of angiotensin converting enzyme inhibitors.
This class of medications are used for several indications and they are:
1) Hypertension,
2) Left ventricular systolic dysfunction,
3) Acute myocardial infarction,
4) In patients who are at high risk of cardiovascular events,
5) In Diabetes mellitus and Renal Failure,
6) Scleroderma Renal Crisis.
To understand why ACE inhibitors can cause dry cough, let us first understand some of the physiology.. (Fig.1)
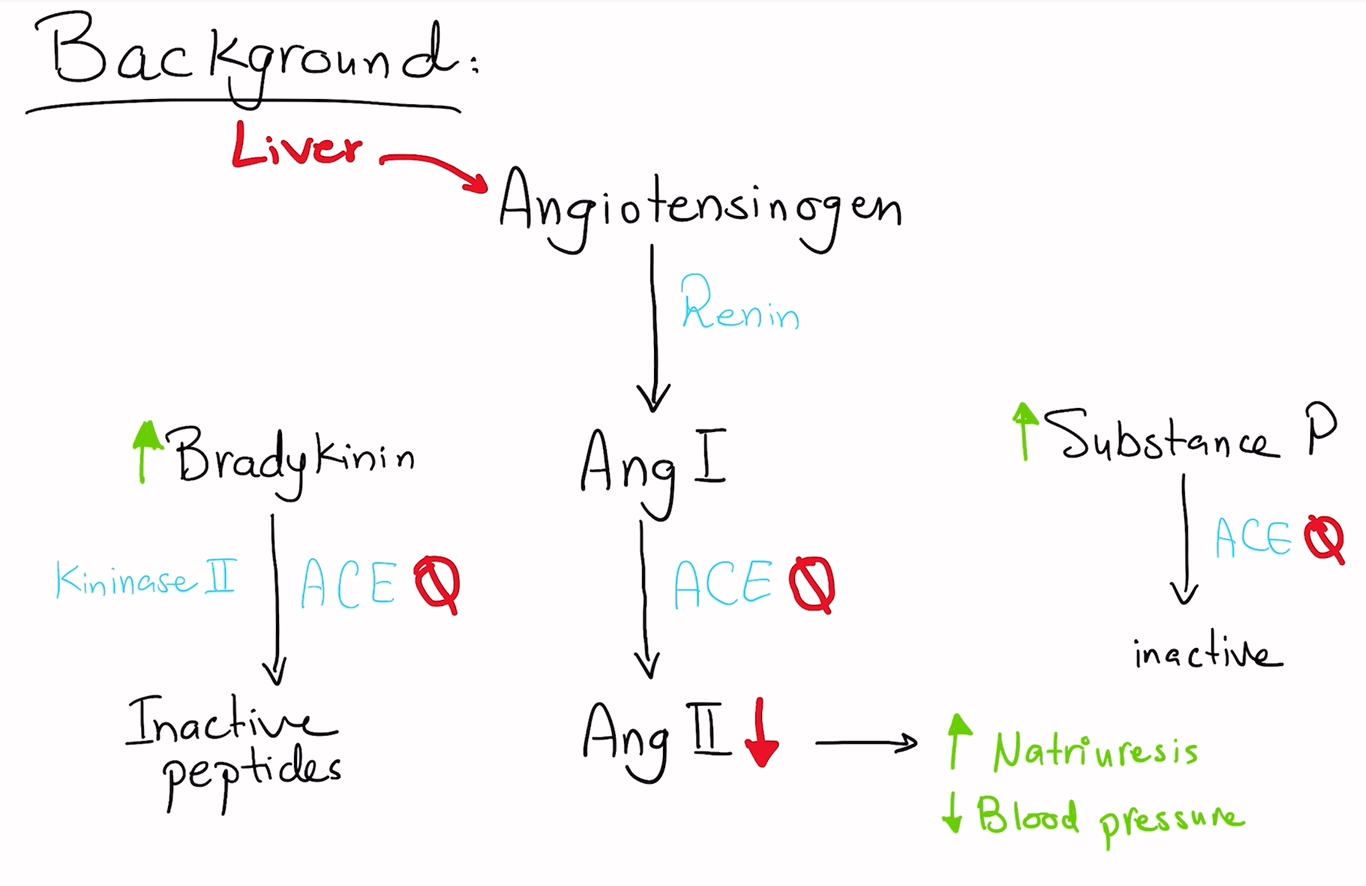
Angiotensinogen, which is primarily produced in the liver, is cleaved by Renin to Angiotensin 1.
And then angiotensin 1 is converted to angiotensin 2 , by the angiotensin converting enzyme (ACE)
ACE also inactivates Substance P.
Kininase II, is the enzyme that inactivates bradykinin and other potent vasodilator peptides. Scientists found that ACE is identical to Kininase II.
Thus, bradykinin is a molecule that is also cleaved by ACE into Inactive Peptides.
So when the ACE inhibitor is administered, it will block cleavage of both Ang I, Bradykinin, and Substance P. (Note that Bradykinin will also induce the release of Prostaglandins)
Inhibition of Ang II production lowers blood pressure and enhances natriuresis.
Inhibition of the degradation of bradykinin has beneficial antihypertensive and protective effects.
On the other hand, The increase in Bradykinin and Substance P levels will lead to the induction of dry cough.
In general ACE inhibitors are well tolerated, however, 5 to 20% of patients can suffer from cough.
The incidence of dry cough in patients receiving ACEIs vary among individual ACEIs, and is the lowest with perindopril. (1) (2)
The onset of ACE inhibitor-induced cough ranges from within hours of the first dose to months after the initiation of therapy. Resolution typically occurs within 1 to 4 weeks after the cessation of therapy, but cough may linger for up to 3 months (3)
So how Bradykinin and Substance P induce the dry cough?
Although the exact mechanism of ACEI-induced cough remains unclear, several theories have been postulated for cough development.
Accumulation of bradykinin and substance P in upper and lower respiratory tracts by ACEIs is the most widely accepted theory.
Bradykinin induces sensitization of airway sensory nerves via rapidly adapting stretch receptors and C-fiber receptors that releases neurokinin A and substance P. This causes airway smooth muscle to constrict leading to bronchoconstriction and cough. However, the reason why cough does not occur in all patients receiving ACEIs still warrants further research. (2)
Another method describes how cough is induced by Bradykinin is the Transient Potential Receptors (TPRs). Several types of TPR ion channels have been described on airway sensory nerves and may be activated by various mediators and physical factors, resulting in cough. TRPV1 (previously called the vanilloid receptor) is activated by capsaicin and bradykinin, all of which are potent tussive agents.
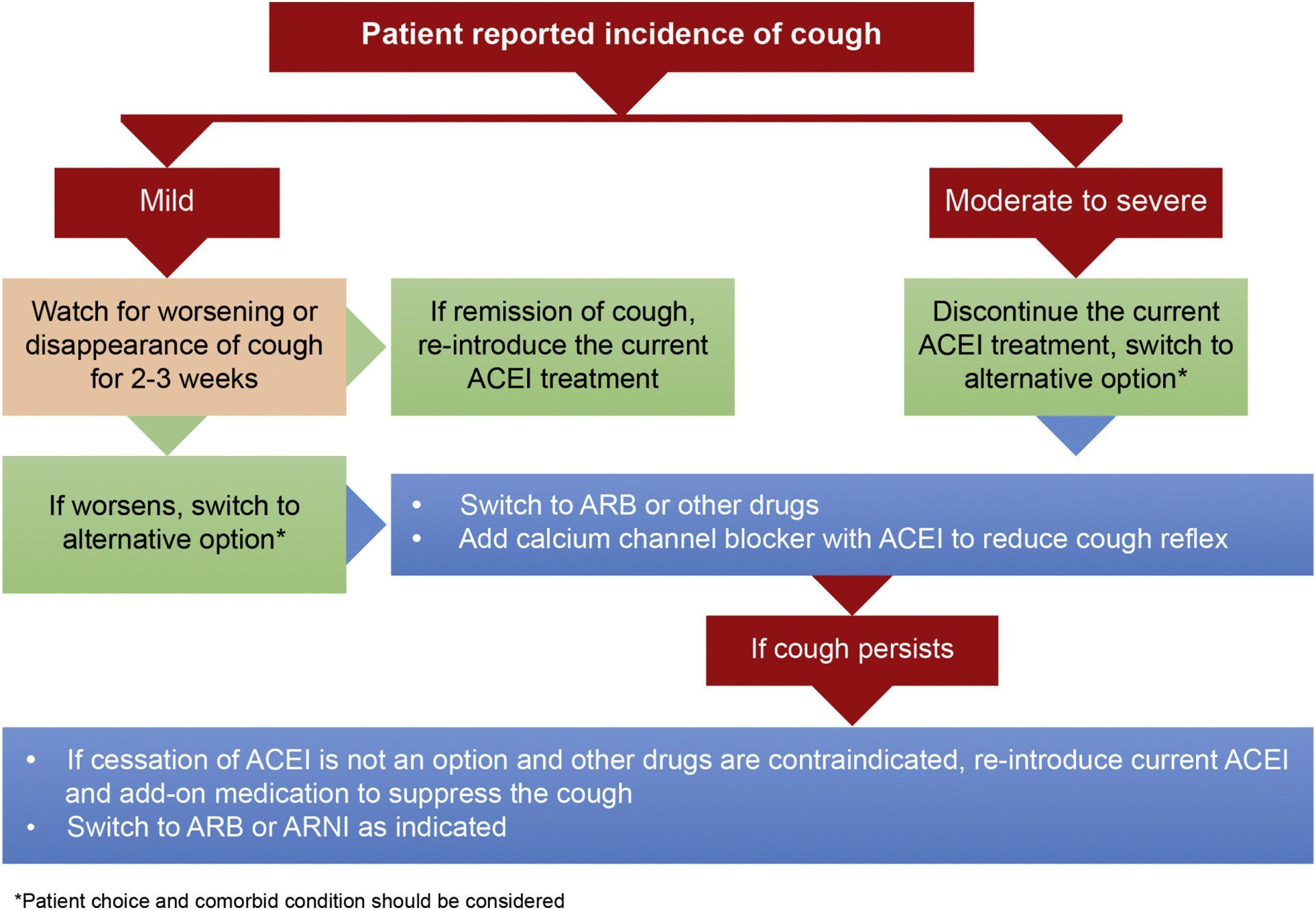
Overall, management of ACEI-induced cough can be done as per this algorithm: (Fig.2)
Other proposed methods to suppress the dry cough?
1) Iron supplementations (4)
2) Thromboxane antagonists, like Picotamide and Aspirin(5)
3) Intermediate but not low doses of aspirin probably can suppress ACEI-induced cough. (6)
4) Calcium channel blockers. (7)
Although it is proven that ACEIs can cause cough, check the results of these two interesting studies:
In a study, for a significant number of patients (27.4%), the cough spontaneously disappeared after 2–8 months of therapy despite continued and unaltered administration of ACEIs and without any therapy aimed for its suppression. All patients were followed up for 13 months after disappearance of cough, and no recurrences were observed. (8)
In another study by the same authors, >50% of patients developed complete resolution of symptoms despite continuing with treatment.(9)
So for sure, additional studies focused particularly on continuation of ACEIs and monitoring the development of cough in patients should be done to conclude and derive recommendations from them.
You can also watch the below video for better understanding of the topic:
Resources:
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7670268/
(2) https://www.sciencedirect.com/science/article/pii/S0019483220301917
(3) https://journal.chestnet.org/article/S0012-3692(15)52845-6/fulltext
(4)https://www.ahajournals.org/doi/10.1161/01.hyp.38.2.166#:~:text=In%20conclusion%2C%20iron%20supplementation%20successfully,activity%20in%20bronchial%20epithelial%20cells
(5) https://pubmed.ncbi.nlm.nih.gov/9217714/
(6) https://pubmed.ncbi.nlm.nih.gov/10933569/
(7) https://doi.org/10.1016/S0011-393X(00)88520-3
(8) https://www.sciencedirect.com/science/article/abs/pii/000291499290630H
(9) https://europepmc.org/article/med/1433168
List of Services
ABOUT THE AUTHOR
Mohamad-Ali Salloum, PharmD
Share
Recent articles: